Reverse ball and socket style shoulder replacements have been around for many decades, but never really caught on due to high failure rates. In other words, we surgeons couldn’t figure out how to make them work right.
However, around the late 1980s, a French surgeon named Paul Grammont figured out the basic biomechanical principles that made the surgery much more successful than it was in the past. Suddenly, we were able to treat conditions that previously had no reliable treatment options thanks to the modern or “Grammont-style” reverse shoulder replacement.
The modern reverse shoulder replacement was FDA approved in the United States in 2004 and since then, shoulder replacement surgery has exploded in popularity. As much as reverse shoulder replacement has been the greatest thing since sliced bread, like any new technology, it also brought with it new complications—one of the most concerning being instability or dislocation.
How the Surgery Has Evolved
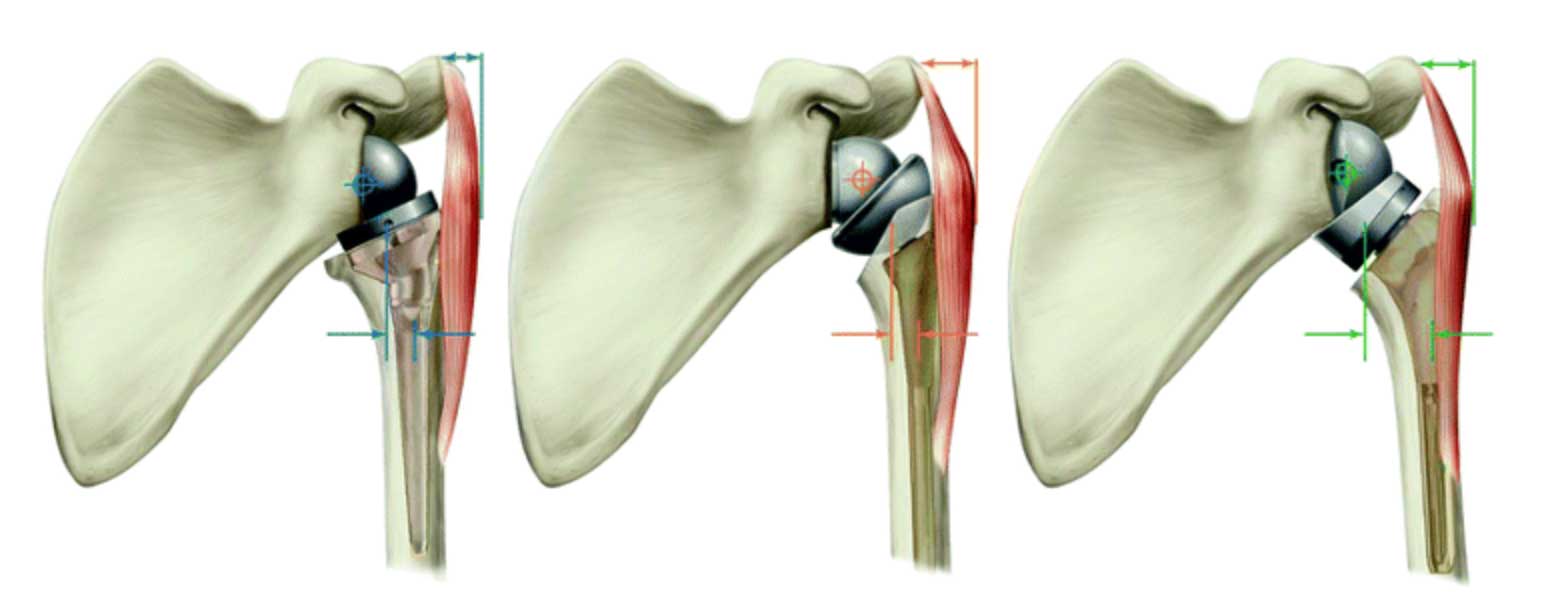
As surgeons did more reverse shoulder replacements, we began to learn more about how we could change the geometry of the prosthesis in order to “rob Peter to pay Paul” and the limits to which we could do so, including:
- How to create a mechanical advantage for rotation or elevation of the arm
- How to increase stability of the prosthesis by changing the size and position of the ball
- How to make up for bone loss of the socket by using bone grafts, wedge shaped implants, or metal augments
- How it could work for conditions other than what it was originally designed for, such as complex fractures
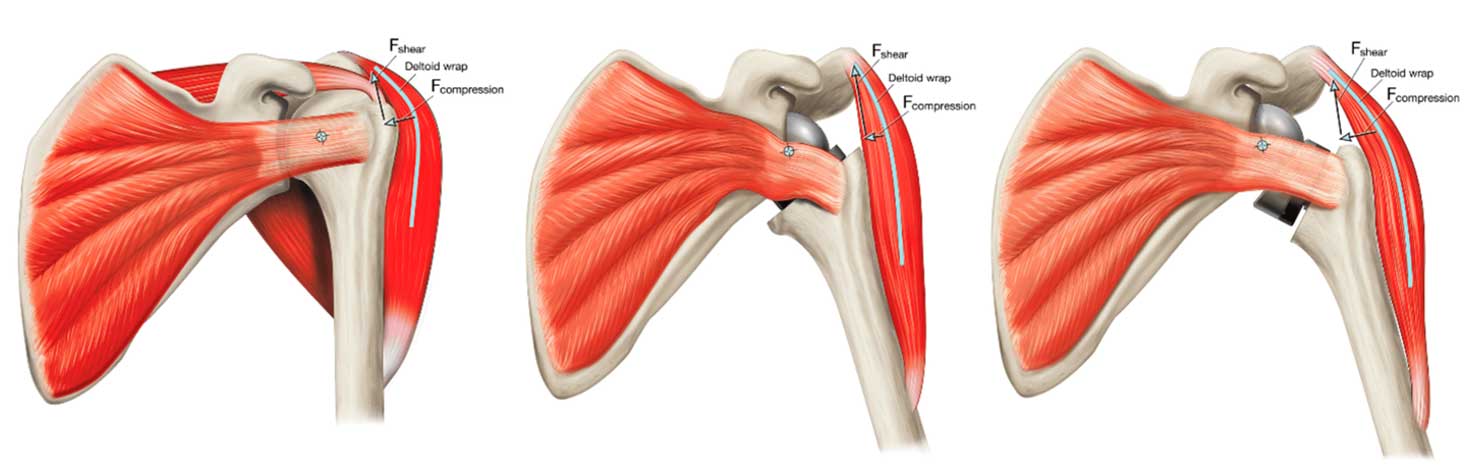
We also began to understand things about the deltoid that we previously hadn’t thought about, including how to make the deltoid work more efficiently, and how it’s primarily responsible for stability in the reverse shoulder replacement (figure 7).
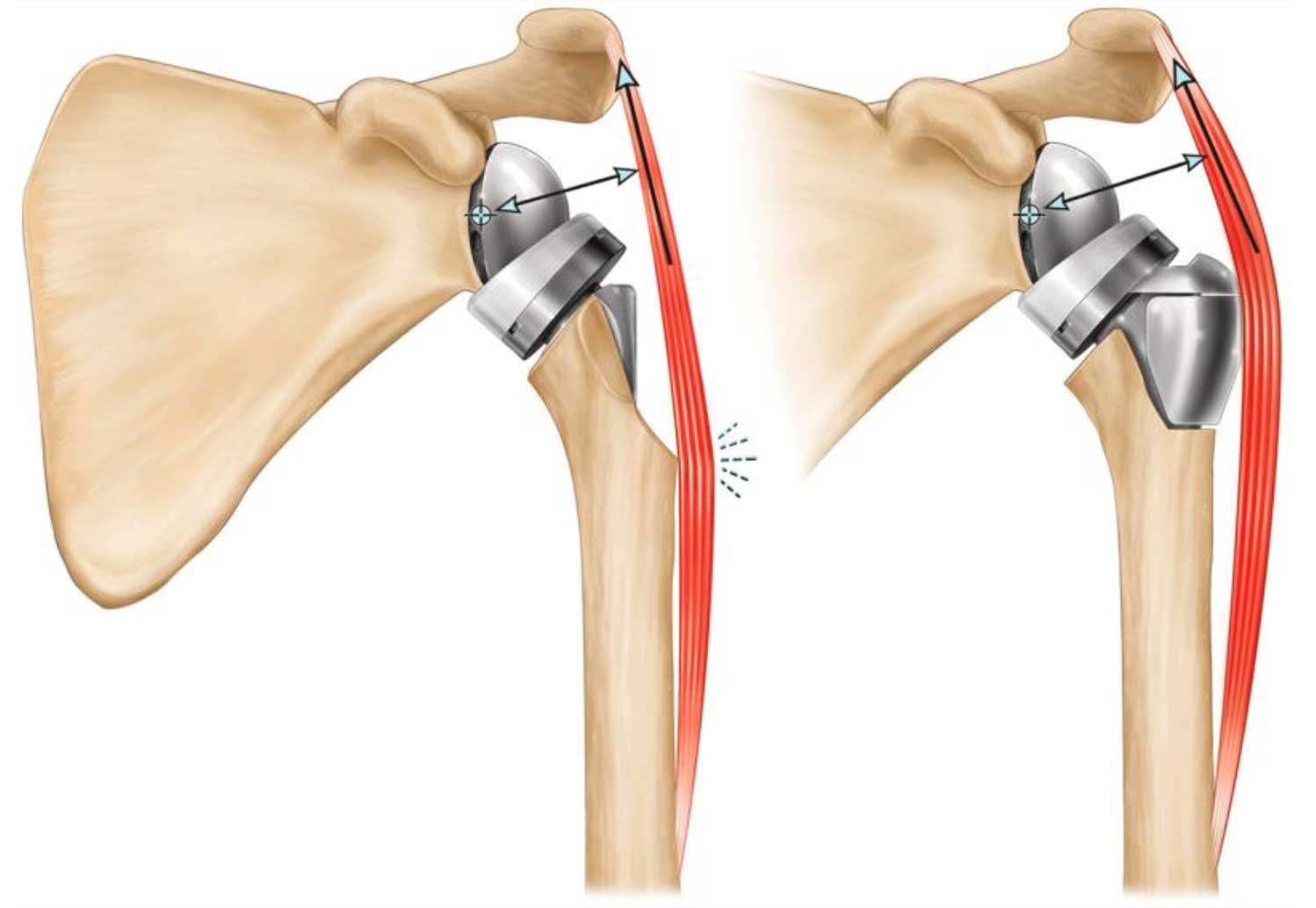
I, as well as others in the field, also started to think about how to make the system even more efficient and more stable than it was previously, as well as how to solve some of the problems with the limits of the reverse we were running into. Specifically, we noticed that patients that were missing the top of the humerus had worse function, were weaker in their ability to lift overhead, and had much higher dislocation rates.
A Point of Clarification
As a point of clarification, it should be noted that although they’re commonly called shoulder replacements, what these surgeries actually do is resurface the shoulder joint, not replace the whole thing. The shoulder is made up of the shoulder blade, or scapula (specifically, the glenoid fossa of the scapula) and the upper arm bone, or humerus. Shoulder replacements don’t replace the whole scapula (or even the whole glenoid fossa) and the whole humerus, they just resurface the articulating surface—the part of one that rubs against the other.
We don’t call them resurfacings because there’s actually a type of shoulder replacement called a resurfacing—which really just confuses things—but in any case, the point is that typical shoulder replacements only resurface the articulating portion of the joint, not the whole thing. There are, however, conditions such as tumors where we do actually replace the entire humerus or the top half or third of it.
Addressing Bone Loss in the Shoulder Socket
What’s actually much more common than having to address bone loss in the humerus is having to address bone loss in the socket, which is most commonly due to the patient simply asymmetrically wearing out the socket (the glenoid fossa) beyond the point of being able to resurface it with a standard prosthetic component.
In order to address this, a company in Florida called Exactech started to make augmented, wedge-shaped prostheses in order to correct for the bone loss of the glenoid that actually worked so well that, nowadays, surgeons are using more augmented glenoid components than standard ones (figure 8).

Augmented prosthesis had been used for many years with great success in the knee and hip to solve problems with bone loss that previously had no reliable solutions, but until only recently no one had done it in the shoulder. At that time, no one made an augment for the humerus, and Exactech was the only company that made augmented glenoid components.
My Work with Exactech
I had already been working with Exactech for several years as a consultant, teaching courses on shoulder replacements, attending meetings, hosting visiting surgeons, advising on complex cases, etc. At one such meeting, a surgeon from Arizona named Matt Hansen proposed a theoretical model of how to increase deltoid efficiency in a rotator cuff deficient native shoulder (one without a shoulder replacement). The basic idea was that since the deltoid elevates the arm by pulling on the humerus you can make the deltoid work more efficiently by having it pull around a corner that basically works as a fulcrum. If you can make a bigger fulcrum by pulling more around the corner you can make the deltoid create more force without doing any more work. Conversely, if the corner is smaller (or missing) then the deltoid generates less force for the given amount of work its doing (figure 9).
As I saw his presentation, I realized that his principle of “supercharging the deltoid”, as it was later called, could be applied to the reverse shoulder replacement, specifically to those patients with proximal humeral bone loss—missing the top of the humerus—in order to solve the problems of weakness and instability in these patients. I immediately began thinking about:
- How to design this
- The practical aspects of manufacturing and distributing it in order to build it as a free-standing prosthesis
- How to install it in a patient that already had a prosthesis without having to remove the old one
- How to make it ambidextrous (using the same implant for right and left shoulders to cut down on manufacturing and inventory)
- How to allow attachment sites for any remaining rotator cuff tendons—and how to make this ambidextrous as well
Within the next few minutes I had a basic design, and at the end of the presentation I went to the chief engineer of Exactech and told him about it. I had literally drawn it—as well as three to five different iterations—on a napkin.
I had proposed design ideas to other companies in the past, many of which said I had an interesting idea, but they were either too busy with higher priority stuff or didn’t think they would sell enough to make it worth their trouble. To my surprise, he asked a few technical questions and said he thought it was a great idea to address a unique problem that no one had a good solution for. He especially liked that, because it was an augment for the humerus and they were the only company that made an augment for the glenoid—it would fit right in with their portfolio.
Over the next few years we had quarterly design team meetings, sometimes in person and sometimes over video call. Another surgeon from Florida, Howard Routman, proposed a similar design. We made several changes, made prototypes, made it in different sizes, tested them in the lab, designed instrumentation to install the device, and applied for a patent on Halloween Day in 2014 and for FDA approval. To our surprise, the FDA approved it on the first application without any significant questions or further testing.
Introducing HAT
The device was eventually called the humeral augmented tray, or “HAT” (although my wife still insists it should be called the “Klug-bump”) and became part of the Equinoxe line of shoulder products from Exactech. The device has been FDA approved for several years now and was officially released in the US on January 1, 2023. It’s now commercially available throughout the US, Japan, and Australia.
To date, about 300 have been put in and I continue to be pleasantly surprised by the feedback I get from surgeons that see the device at meetings and are performing the procedure. I believe we now have eight patents on it—in the US, Spain, Australia, Japan, Europe, World, Brazil, and Canada. I look forward to seeing how the patients are doing with this unique device over the years.
Overall, the experience of designing a medical device has been incredible. It was tons of fun and also very rewarding and reassuring to see that others—as well as industry—have embraced an idea that I thought would help patients and solve a unique problem that we didn’t really have a great solution for in the past. I look forward to further design projects and hopefully can contribute more in the future to solving more of the unsolved problems in shoulder and elbow surgery.
Read the first post on Shoulder Replacement Surgery
If you think you need or are interested in learning more about shoulder surgery—including a reverse shoulder replacement—we’re happy to help. Please reach out to book an appointment with Dr. Klug.

